Spasticity is a condition characterized by muscle stiffness and involuntary contractions, often occurring in individuals with neurological disorders such as multiple sclerosis (MS), cerebral palsy (CP), stroke, or spinal cord injury (SCI). While spasticity can pose significant challenges to mobility and quality of life, understanding its causes, symptoms, and management options can empower individuals to navigate these challenges effectively.
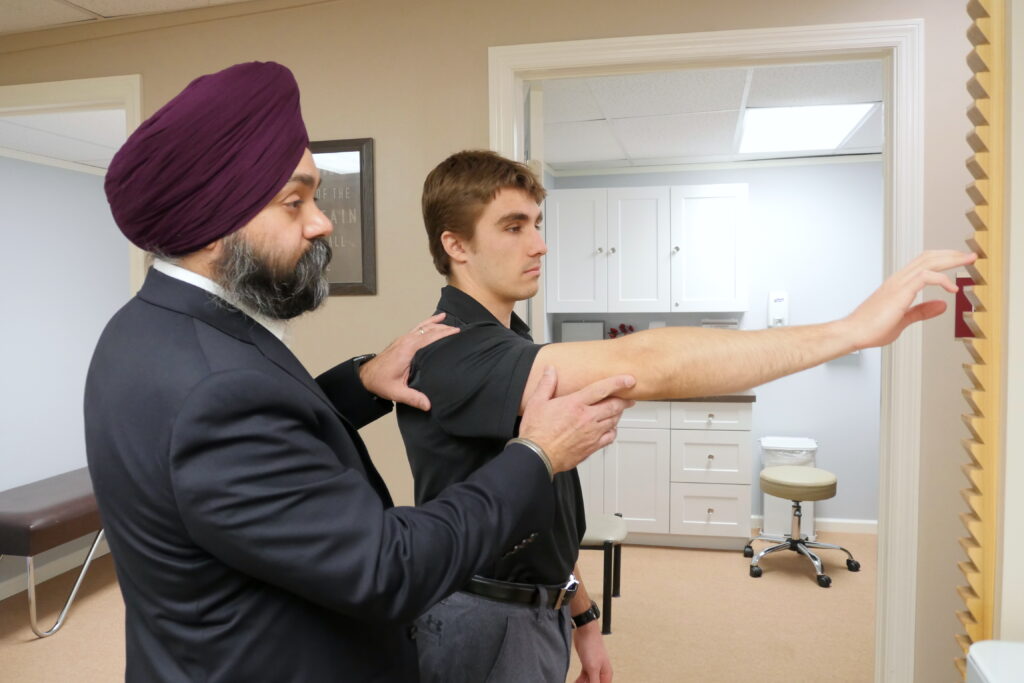
- Physical Therapy: Exercises and stretches are tailored to improve range of motion, muscle strength, and flexibility while minimizing spasticity-related discomfort.
- Medications: Oral medications like muscle relaxants or anti-spasticity drugs may be prescribed to manage spasticity. These can include Baclofen, Diazepam, or Tizanidine, among others.
- Injections: Botulinum toxin injections (e.g., Botox/Dysport/Xeomin) are commonly used to selectively weaken overactive muscles and reduce spasticity.
- Orthotics and Assistive Devices: Braces, splints, or orthoses may be recommended to support affected limbs and improve function.
- Intrathecal Baclofen Therapy (ITB): For severe cases, a pump can be implanted to deliver Baclofen directly into the spinal fluid, providing targeted relief from spasticity.
- Surgical Interventions: In some instances, surgical procedures like selective dorsal rhizotomy or tendon release may be considered to address severe spasticity.
- Follow-Up and Monitoring: Regular follow-up appointments are crucial to assess progress, adjust treatments, and address any new concerns.
- Patient Education and Support: Providing education and support to patients and their caregivers is essential for understanding the condition, adhering to treatment plans, and maximizing outcomes.
Overall, the goal of spasticity management in physical medicine and rehabilitation is to improve quality of life, enhance functional abilities, and promote independence for individuals living with spasticity.